HH Newspost – Mary McNeil
Congratulations to Holland Home resident, Mary McNeil, who received the ‘Volunteer of the Year Award’ from LeadingAge Michigan. To learn more about this incredible recognition, click on the link. […]

Check here for the latest information and updates.

Congratulations to Holland Home resident, Mary McNeil, who received the ‘Volunteer of the Year Award’ from LeadingAge Michigan. To learn more about this incredible recognition, click on the link. […]

At our recent resident panel event, prospective residents were able to hear from current residents about the how and why behind their decision to move into Holland Home. In this post, we recap some of the main takeaways. […]
Read More… from Resident Panel Recap: Exploring the Decision to Move
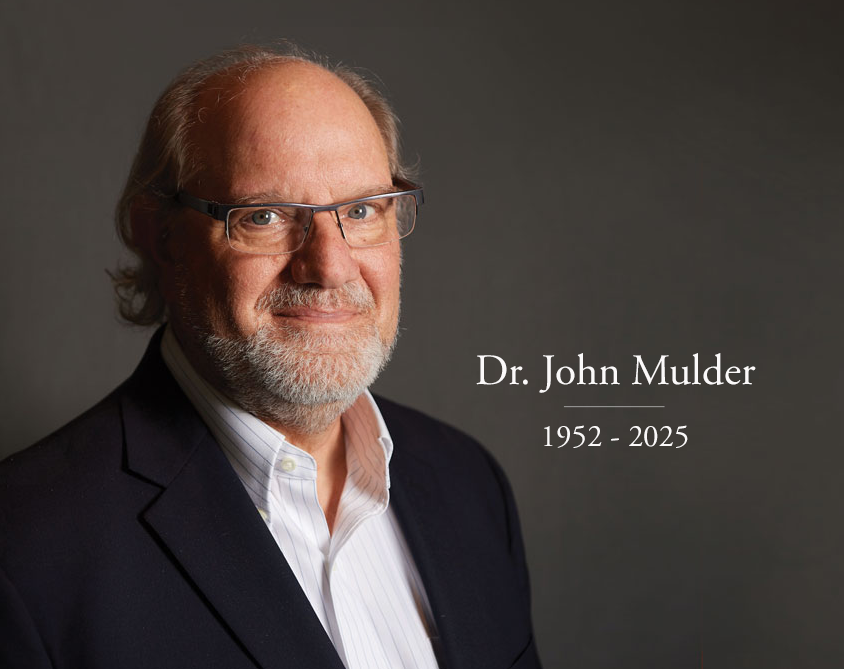
It is with deep sadness that we share the news of the passing of Dr. John Mulder, former Medical Director of Faith Hospice and Executive Director of Trillium Institute. Dr. Mulder has left an indelible mark on the field of hospice and palliative care and on our community. Our thoughts and prayers are with his loved ones during this difficult time. To learn more about his impact as a physician, educator, and friend to many, please click on the link below. […]
Read More… from Honoring the Life & Legacy of Dr. John Mulder

Advance care planning provides peace of mind by ensuring that loved ones’ wishes are honored and families are prepared when the time comes. Thoughtful planning allows you and your loved ones to make informed decisions about future care, reducing stress and uncertainty. In this blog, learn how you can start initiating conversations and planning for the unexpected. […]

As a Continuing Care Retirement Community (CCRC), Holland Home provides a full continuum of care, ensuring that residents have access to higher levels of support if their needs change, even if they outlive their financial resources. In our latest blog, we recap our Care Navigation Webinar and share how residents can transition through the different levels of care. Read now in this blog!
[…]
As a locally-owned and operated nonprofit, Holland Home’s priority is the people we care for, not shareholders or bottom-line growth. In this blog, learn more about the benefits of being a locally-owned, mission-driven organization. […]
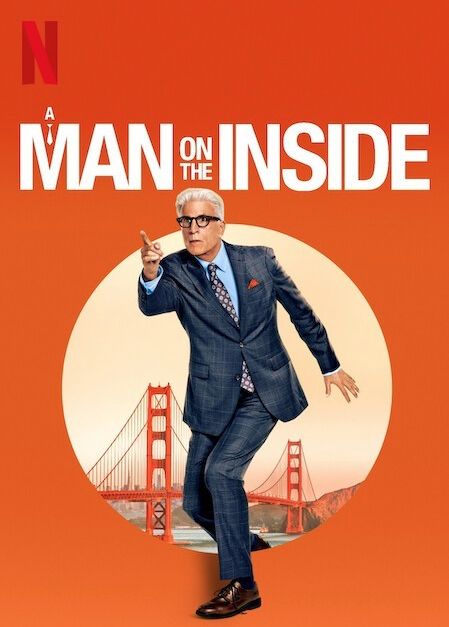
A Man on the Inside touches on important themes of loneliness, isolation, and friendship for aging adults, sparking important conversations in an approachable and light-hearted way. So, what exactly does the show get right about senior living? We break it down, with spoiler alerts, in this blog. […]
Read More… from What does Netflix’s hit show get right about senior living?

As you consider a move to senior living, one of the more intimidating tasks to complete is downsizing and selling your home. Whether you’re planning for the future or have already started the process, understanding the current real estate market and preparing your home for sale is an important step in the process.
We recently hosted Michael Courtright of Greenridge Realty on our At Home with Holland Home webinar series, and we’re recapping his important insights in this blog.
[…]
Read More… from Selling Your Home and Investing in Senior Living

We always stress the importance of planning ahead, especially when it comes to your future and senior living. And the cold, gloomy days of winter provide the perfect opportunity for planning and organizing. In this blog, we’re sharing a few tips to help people who are starting to plan for their next chapter in a senior living community. […]

In this episode, we dive into a reality that’s becoming all too familiar for today’s sandwich generation: balancing careers, young families, and the growing needs of their aging parents. For many adult children, this journey is filled with complex decisions, emotions, and unknowns. Our guest, Diane Lobbestaal, faced these same challenges while caring for her aging parents. She joins to share her journey, shedding light on the guidance, care, and compassionate support system available to them. […]

From social connection to safety and opportunities for personal growth, senior living communities offer a lot of benefits for single aging adults. We understand it can be hard to think about leaving behind your familiar environment and stepping into a new place with new people, but the supportive, welcoming community that awaits at Holland Home is well worth the change. […]
Read More… from The Benefits of Senior Living for Single Older Adults

The cost of a senior living community plays a huge role in a prospective resident’s decision-making process. “Can I afford it? Is it worth the investment? What does it mean for the legacy I will leave behind?” Learn more about the costs and benefits of Holland Home in this blog. […]